IVF treatment and process
What is IVF?
IVF (In Vitro Fertilisation) is a procedure, used to overcome a range of fertility issues, by which an egg and sperm are joined together outside the body, in a specialised laboratory. The fertilised egg (embryo) is allowed to grow in a protected environment for some days before being transferred into the woman's uterus increasing the chance that a pregnancy will occur.
In Vitro Fertilisation (IVF) can be used to overcome a range of fertility issues and for many couples, gives them the best chance of having a baby.
Enquire Today
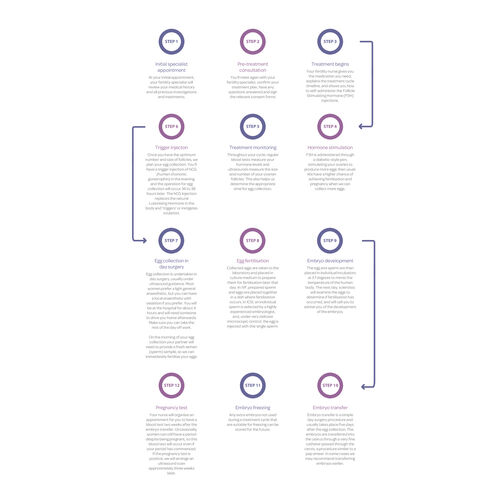
The IVF process step by step
Your treatment will be coordinated by your fertility specialist who is supported by an experienced team of nurses, counsellors and scientists. We understand how important having a family is to you and can assure you that we will provide you with the highest standard of fertility care.
Below is an outline of the steps you can expect during your IVF journey.
Step 1: Initial specialist appointment
At your initial appointment, your fertility specialist will review your medical history and conduct the following tests to provide preliminary advice about your treatment options.
- Blood tests: This includes antenatal testing, Anti Mullerian Hormone (AMH), hormonal profile (pituitary, ovaries and thyroid) and Karyotype (checking chromosome - genetic material) to make sure the number of Chromosomes is correct and that they are in the right order.
- Pelvic ultrasound: To get an idea of the structure of the pelvis, the uterus and what it looks like, the ovaries and their positioning and if there are any problems that require further investigation.
- Semen analysis: If your male partner is present, he will undergo a semen analysis to make sure there’s enough good quality swimmers. They specifically look at shape, size, count and movement.
Step 2: Pre-treatment consultation
After your initial appointment, you’ll typically meet again with your fertility specialist for a follow-up consultation, where you will receive your results. Based on these results, your doctor will create a treatment plan that is most appropriate for your situation.
Normally, a nurse orientation appointment is also arranged for you at the clinic, to run through the full process and what to expect. Your fertility nurse gives you the medication you need, explains the treatment cycle timeline, and shows you how to self-administer the Follicle Stimulating Hormone (FSH) injections. We recommend both you and your partner attend this appointment.
Step 3: Treatment begins
There are multiple ways of stimulating your ovaries for the purposes of IVF. The antagonist protocol is the most used protocol, the timing of which is outlined below.
Day one of IVF treatment is considered to be the first day of your menstrual cycle. When you get your period, you’ll need to call the nurses to let them know. You will normally come in on Day 2 to begin hormonal stimulation.
Step 4: Hormone stimulation
You will administer these injections yourself through a diabetic-style pen to stimulate your ovaries to produce more eggs than usual. After five days, you will return to your clinic to understand how your body has responded to the injections (to avoid under or over-stimulating the ovaries). We have a higher chance of achieving fertilisation and pregnancy when we can collect more eggs.
Step 5: Treatment monitoring
If you are on track with your FSH injections, you will undergo a follow-up ultrasound scan and blood test to confirm your body is heading in the right direction (stimulation) for your IVF cycle. This also helps us determine the appropriate time for egg collection. All your blood and ultrasound tests are conducted by our nurses within your chosen IVFAustralia clinic and are included as part of your treatment costs.
Step 6: Trigger injection
Once you have the optimum number and size of follicles, we plan your egg collection. You’ll have a trigger injection of hCG (human chorionic gonatrophin) in the evening, and the operation for egg collection will occur 36 to 38 hours later. The hCG injection replaces the natural Luteinising Hormone in the body and 'triggers' ovulation so that the eggs mature and become ready to be collected.
Step 7: Egg collection
Two days later, you will attend the day surgery to undergo an egg retrieval (this is the only day you will need to take off work during your IVF cycle). The procedure takes around 20-30 minutes; you will be completely asleep whilst your fertility doctor uses a thin needle through the wall of the vagina to drain the follicles, guided by an internal scan. When you have recovered from the procedure, you will be advised as to the number of eggs collected.
It's likely you will be at the hospital for about 4 hours and will need someone to drive you home afterwards. If your partner is supplying the semen sample, he will do so on the morning of your egg collection so we can immediately fertilise your eggs.
Step 8: Egg fertilisation
Following your egg collection, your eggs are immediately transported to the laboratory, where your eggs and your partner, or donor’s, sperm are placed together in a dish where fertilisation occurs. If there is any concern about sperm quality, the process of fertilisation is carried out by Intracytoplasmic Sperm Injection (ICSI). This is where one sperm is inserted into each egg.
After the eggs and sperm have been assessed, you will typically receive a call from the laboratory with an update.
Step 9: Embryo development
The next day, scientists will examine the eggs to determine if fertilisation has occurred. We usually grow embryos in the laboratory until Day 5, known as the Blastocyst stage, because there is strong evidence that these embryos are more likely to implant in the uterus. A Blastocyst is the optimal stage of development for an embryo; ‘blast’, meaning ‘making’, and cyst, meaning ‘a pool’, which essentially mimics a visual of this stage of development.
Step 10: Embryo transfer
Embryo transfer is a simple day surgery procedure and usually takes place five days after the egg collection. The highest quality embryo is transferred into the uterus through a very fine catheter passed through the cervix, a procedure similar to a cervical screening. In some cases, we may recommend transferring an embryo earlier.
Step 11: Pregnancy test
Your nurse will organise an appointment for you to have a blood test two weeks after the embryo transfer. Occasionally, women can still have a period despite being pregnant, so this blood test will occur even if your period has commenced. We do not recommend using urinary pregnancy test kits, as the hormone medication given throughout treatment could produce an incorrect reading.
Your pregnancy blood test results are usually available by mid-afternoon. If the pregnancy test is positive, we will arrange an ultrasound scan approximately three weeks later.
Ready to start your IVF journey?
Begin your journey with IVFAustralia by requesting an appointment with one of our leading fertility specialists. Initial consultations can be face to face or online, depending on your Doctor and what works for you.
Call our friendly team on 1800 111 483 to learn more about getting started, or fill out the form below. We are committed to supporting you throughout your journey and can help with any questions you might have.
IVF Treatment and Process FAQs
What does IVF stand for?
IVF stands for In Vitro Fertilisation, in vitro meaning ‘in the dish’ and fertilisation, which takes place outside of the body.
How much does IVF treatment cost?
The cost of IVF in NSW IVF cycle payment Estimated out of pocket costs for an initial cycle in a calendar year Estimated out of pocket costs for a subsequent cycle in a calendar year $11,566 $6,029 $5,346 Read more about the costs of fertility treatment and payment options at IVFAustralia.
What does the Medicare safety net mean?
Once you reach the Medicare Safety Net threshold in a calendar year, Medicare will pay an additional rebate on selected items. In a calendar year, generally during your first IVF cycle, you can expect your out-of-pocket costs to be approx. $6,029.
If you need more than one cycle in a calendar year and reach the Medicare safety net, your out-of-pocket costs will be less at $5,346.
What is IVF pregnancy?
A successful IVF pregnancy is the desired outcome of the IVF process, which is primarily used to treat infertility. Unlike a natural pregnancy, an egg and sperm are joined together outside the body in a specialised laboratory. The fertilised egg (embryo) grows in a protected environment for some days before being transferred into the woman's uterus, increasing the chance that a pregnancy will occur.
How is IVF done?
In short, the IVF process begins with stimulating the ovaries for around two weeks to create multiple eggs. Once the ovaries have been stimulated to produce these eggs, a fertility doctor surgically removes the eggs and adds them to a dish with sperm in hopes that the eggs will fertilise and, over a five-day period, develop into embryos.
Video: How IVF treatment works
How long does IVF take from the first appointment?
Starting your IVF cycle can vary depending on when the treatment plan is confirmed and when your period begins. From Day 1 of your period, each IVF treatment cycle takes around four to six weeks. While the length of each IVF step can vary, below is an example of a standard IVF treatment cycle timeline.
What day of your cycle do you start IVF injections?
Depending on your individual circumstances, treatment begins on the first day of your period. Whether you’re going ahead with ovulation tracking, IVF or IUI this is the first day of your cycle and a sign to commence treatment.
Can you choose gender with IVF?
Gender selection during IVF treatment is not legally allowed in Australia due to the ethical, legal and social issues it raises. In Australia, gender selection is only available if it is required to prevent certain genetic disorders which would only affect one gender. It is not available for family balancing.
How many injections for IVF treatment?
On average, IVF patients will receive 1–2 injections per day. The first injection is an FSH injection, which stands for Follicle Stimulating Hormone. You administer these injections yourself for the next five days, then return to your clinic to understand how your body responded to the injections. The nurses will then recommend either increasing or decreasing the number of injections depending on how your body has responded to it.
Does IVF hurt?
While this largely depends on your pain tolerance, most women do not find IVF treatment painful, and you should never be in extreme pain. However, discomfort caused by side effects like abdominal cramping, bloating or breast tenderness can occur during different phases of the IVF process due to the injections and fluctuation in hormones. During procedures like egg retrieval, anesthesia is used to help ensure a pain-free experience and over-the-counter medications are recommended to ease any discomfort.
How does frozen embryo transfer work in the IVF timeline?
During the IVF process, there is a 5-day period where embryos develop into blastocysts. If more than one healthy embryo develops during this timeline, the extra embryo(s) can often be frozen and stored for future use in subsequent cycles.
Are the steps in the IVF treatment process always the same?
IVF treatment is tailored to your specific needs by your fertility specialist. Most patients who undergo IVF will be prescribed one of two main treatment protocols, Long Down Regulation or Antagonist treatment cycles.
Want more information?
To find out more about what’s involved in IVF treatment please come to a free information night or book an appointment with a fertility specialist. Appointments are available and will cost approximately $200 for a couple after the Medicare rebate.
- Find out more about IVF success rates
- Learn about other Fertility Treatments
- Understanding Infertility
- Learn more about the IVF journey with the Big Miracles docuseries
Recommended Reads
At IVFAustralia, we’re here to help you navigate every step of the IVF journey with confidence and understanding. Dive deeper with valuable insights, expert guidance, and empowering stories.

Self care during IVF treatment
Looking after your emotional health is just as important as what’s going on physically in an IVF cycle. The frustrations of infertility can place strain on mental health and relationships. Read our tips for self care here.

Managing relationships during IVF
Struggling to conceive is tough enough, but maintaining relationships while undergoing the ups and downs of fertility treatment has its own set of challenges.

Big Miracles: IVF Documentary Series
Big Miracles is a documentary series available on 9Now, capturing the candid moments of real Australian couples going through IVF and other fertility treatments. The show, filmed within IVFAustralia clinics, reveals an inside look into the complexities of fertility treatment, from seeing specialist pre-treatment consultations,the fateful egg collection and laboratory process.